This week, thousands of experts from around the world will gather at the American Society of Nephrology (ASN) annual meeting and science exposition to share insights on current issues and developments related to kidney disease. According to ASN, kidney disease affects 850 million people globally, can lead to significant morbidity and mortality, and creates a large financial burden on patients and society. Here, we explore the impacts of chronic kidney disease (CKD), and why they make it imperative to develop better and more accessible methods of diagnosis and treatment.
Diagnosing CKD
In the US, the CDC reports 35.5 million adults, or roughly one out of seven, have CKD.1 Despite these high rates, an estimated 90% of those affected do not know that they have it. This is primarily due to the lack of noticeable symptoms in many patients because of the kidney’s ability to compensate for abnormal function in the earlier stages of disease. Later, symptoms may be somewhat nonspecific and mostly related to fluid retention or absorption/excretion issues: weight loss, poor appetite, tiredness, shortness of breath, cramps, headaches, sleep disturbances, to name a few. Blood in the urine (hematuria) may also be seen, which may trigger concern. Although these factors can make it difficult to identify signs of CKD in early disease, early diagnosis can enable improved outcomes through more timely intervention and informed disease management.
Risk factors for CKD
There are several risk factors for CKD that have been identified, both physiological and demographic. The National Kidney Foundation indicates most kidney disease is related to diabetes and hypertension, though obesity can also play a role.2 Diabetes and hypertension are two prevalent, chronic conditions in the general population and known for having challenges to their management which, over time, often lead to impacts on kidney function.
Percentage of US Adults Aged 18 Years and Older With CKD, by Age, Sex, and Race/Ethnicity (CDC)
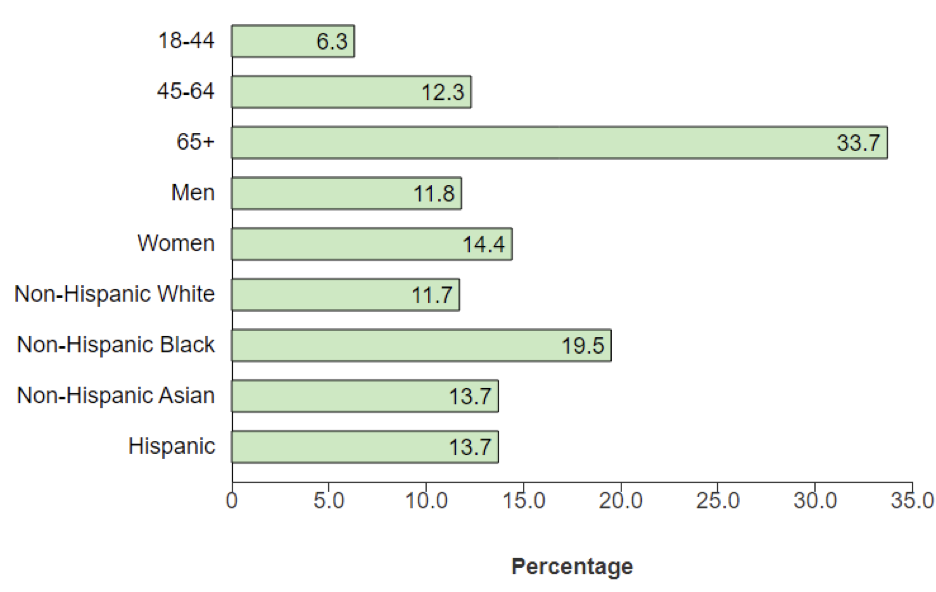
Additionally, race and ethnicity play a notable role in CKD risk and outcomes. Compared to white patients, Black patients have been found to have four times the risk of kidney failure, as well as higher levels of concurrent diabetes and hypertension. Hispanic patients also have higher rates of negative outcomes, with about double the risk of kidney failure as white patients. And while, in general, annual mortality among those with CKD is double the rate of those without it, CKD mortality is greater among Black and Hispanic populations. These statistics emphasize the importance of developing CKD treatment that is accessible to all populations, as well as capable of addressing and mitigating such severe negative outcomes.
Costs of CKD
As an ongoing condition, CKD requires ongoing treatment. However, the costs and accessibility of such treatment can be quite high. Although health insurance can help to bear much of the cost of care, access to healthcare may be limited for some communities. For instance, among the demographics most at risk for kidney failure from CKD, about 33% of Hispanic populations and 20% of Black populations are uninsured, leaving these patients with little economic recourse for costly treatments.2 Nevertheless, regardless of demographic, the high cost of chronic care can impact a person’s access to consistent CKD management, increasing risks to their health.
Among those who are insured, approximately 64% of new kidney failure patients are enrolled in Medicare, meaning the high costs of CKD are borne societally as well. In 2018, Medicare costs associated with kidney disease were $130 billion.2 As kidney disease progresses and advanced therapies — such as hemodialysis, peritoneal dialysis, and transplantation, with annual costs of $93000, $78000, and $37000 respectively — become necessary, Medicare becomes an important mechanism for medical reimbursement.
The importance of kidney disease research
Kidney disease has major impacts on the health of a large segment of the global population. Recognizing risk factors and observing for onset of kidney disease so there can be early intervention or preventive measures taken are important for mitigating the longer-term consequence of kidney failure. This is especially true of community awareness efforts, diabetes and hypertension screening, and targeted efforts in certain higher risk demographic groups. Sharing information related to these efforts plus new approaches to diagnostic testing and therapy (preventive and interventional) is important to assist healthcare professionals develop a sound plan for the patients they see in practice.
As evidenced by the thousands of experts participating in Kidney Week, many nephrologists and their colleagues are dedicated to improving CKD care. Even so, advancing the necessary diagnostics and therapies will likely take years of concentrated efforts in kidney disease research. By developing safe, accessible treatments backed by real world evidence, we can improve the lives of millions of people around the world.
References
- CDC. “Chronic Kidney Disease.” Chronic Kidney Disease, 21 May 2024, https://www.cdc.gov/kidney-disease/index.html.
- Kidney Disease: Fact Sheet | National Kidney Foundation. https://www.kidney.org/about/kidney-disease-fact-sheet. Accessed 22 Oct. 2024.
About UBC
UBC is the leading provider of evidence development solutions with an expertise in uniting evidence and access. UBC helps biopharma mitigate risk, address product hurdles, and demonstrate safety, efficacy, and value under real-world conditions. Bringing over 30 years of experience, UBC is uniquely positioned to develop diversity action plans, end-to-end integrated evidence generation strategies, identify fit-for-purpose data sources, operationalize planned studies, and ensure regulatory-grade, publishable outputs.
About the Author

BRUCE SMITH, PHARMD
Executive Director – Clinical Strategy
Dr. Smith has had a 43-year career in academic medicine and drug development. Thirty-four of these have been spent in the contract research environment, including 20 at UBC. Dr Smith has worked, in various operational and scientific leadership positions spanning phases I-IV clinical trials, observational studies, real world evidence, and expanded access. He has published over 100 papers in refereed journals, been a member of editorial boards, and session chair and speaker at national and international medical conferences. He brings unique perspectives from his experiences interacting with patient groups, health authorities, NGOs, academic leaders, and other stakeholders in 50 countries.